Abstract
Background: Sickle cell disease (SCD) is documented to be a key driver of adult hospitalizations, high length of stay, and frequent ED utilization at urban hospitals. In FY16 the average length of stay (ALOS) for adult SCD inpatient encounters at Virginia Commonwealth University Medical Center, an urban tertiary care center containing an adult SCD center, was 6.7 days, compared with an expected ALOS of 4.2 days. The 30-day readmission rate for SCD was 33.7%. Therefore, in an effort to reduce acute care utilization and re-hospitalization for VCU SCD adults, substituting it with ambulatory care and a medical home, we conducted a pilot study.
Methods: we implemented Multidisciplinary Adult Care and Instrumental Support (MAIS), a form of the patient-centered medical home, for 5 of the highest SCD adult utilizers, among approximately 500 adults with SCD. There was not a control group. We hired and trained special SCD community health workers, labelled Patient Navigators (PNs), as case managers. PNs coordinated care with adult sickle cell providers, who customized medical interventions according to patient characteristics and needs discovered by PNs. PNs also coordinated care with hospitalists, ED physicians, social workers, mental health providers, and community resources. Issues addressed by PNs included housing, severe mental health and cognitive impairment, educational barriers, transportation barriers, poor ADL skills, domestic violence & stalking, and lack of family support. Analysis used a before-after design.
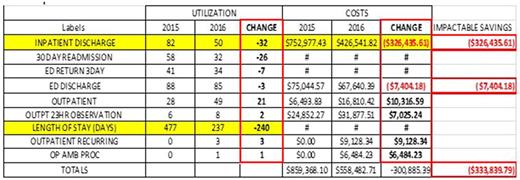
Results: Included very high utilizing patients were ages (21 to 29), 2 were male and 3 were female. Insurance coverages included Medicaid, Medicare, Anthem health keepers and Optima Health. All 5 patients had multiple issues contributing to their high utilization. The 5-patient pilot evaluation showed a 1-year savings of $333,839, a 35.01% improvement for these 5 patients, calculated using the CMS percent change methods (($558,482.71 - $859,368.10)/$859,356.10X100). Additionally, 30-day readmissions were reduced by 18.4%, ALOS was reduced by 1.2 days, and the number of SCD clinic appointments doubled. The table shows savings in discharges, readmissions, and LOS, as well as increases in ambulatory care, for these patients.
Conclusions/Future work: We conclude, in an uncontrolled pilot, there were dramatic reductions in hospital costs, discharges, readmissions, and length of stay, as well as increases in ambulatory care, resulting from using MAIS. Our pilot adds support to a growing body of data suggesting that a substantial case management support structure as part of a patient-centered medical home can reduce the risk of repeated ED visits, hospitalization, and lengthy stay in adults with chronic disease. Future work should include more rigorous evaluations, including costs of the program, control group comparisons, and return on investment, and should test whether this approach may complement or may be used instead of other approaches to improve LOS, readmission rates, and cost of care in SCD.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal